Gangrene In Special Populations: Understanding Risk Factors And Challenges
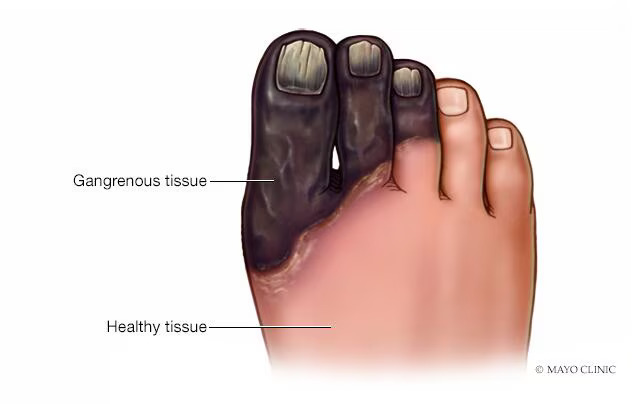
Gangrene, a condition characterized by tissue death due to reduced blood supply or bacterial infection, poses significant risks and challenges, particularly in certain special populations. Individuals with specific medical conditions or lifestyle factors may be at higher risk of developing gangrene, and they may face unique challenges in diagnosis, treatment, and management. In this article, we will explore gangrene in special populations, including the risk factors, challenges, and strategies for prevention and care.
Risk Factors for Gangrene in Special Populations
Certain special populations are at increased risk of developing gangrene due to various factors, including:
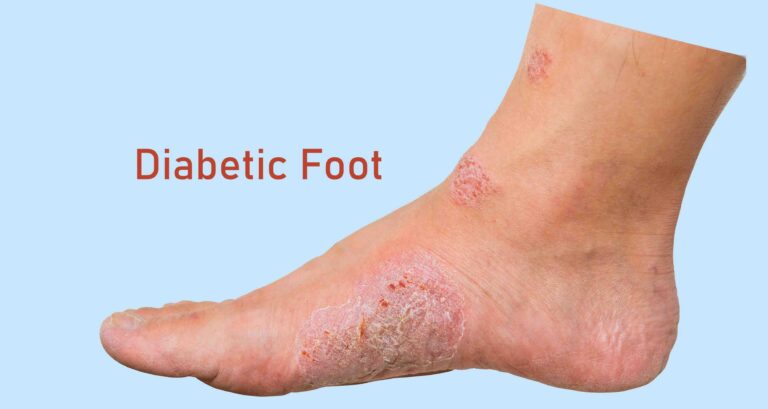
- Diabetes Mellitus:
Individuals with diabetes mellitus are particularly susceptible to developing gangrene due to complications such as peripheral neuropathy and peripheral vascular disease. Peripheral neuropathy reduces sensation in the extremities, making it difficult for individuals to detect injuries or infections that can lead to gangrene. Peripheral vascular disease impairs blood flow to the extremities, increasing the risk of ischemic gangrene. - Peripheral Arterial Disease (PAD):
Peripheral arterial disease, a condition characterized by narrowed or blocked arteries in the legs, increases the risk of ischemic gangrene. Reduced blood flow to the extremities can result in tissue necrosis and gangrene, particularly in individuals with advanced PAD or other cardiovascular risk factors. - Elderly Population:
The elderly population is more vulnerable to gangrene due to age-related changes in circulation, immune function, and tissue integrity. Chronic medical conditions, such as diabetes, cardiovascular disease, and peripheral neuropathy, further increase the risk of gangrene in older adults. - Immunocompromised Individuals:
Immunocompromised individuals, including those with HIV/AIDS, cancer, organ transplantation, or autoimmune disorders, are at increased risk of developing infectious gangrene. Impaired immune function predisposes these individuals to bacterial infections that can lead to tissue necrosis and gangrene. - Trauma and Injury:
Individuals who have experienced trauma or injury, such as crush injuries, fractures, or burns, are at higher risk of developing traumatic or ischemic gangrene. Trauma disrupts blood flow and tissue integrity, increasing the likelihood of tissue necrosis and subsequent gangrene.
Challenges in Diagnosis and Management
Special populations facing gangrene encounter unique challenges in diagnosis, treatment, and management:
- Delayed Presentation:
In certain special populations, such as the elderly or individuals with neuropathy, gangrene may go unnoticed or present atypical symptoms, leading to delays in diagnosis and treatment. Delayed presentation increases the risk of complications and may necessitate more aggressive interventions. - Complicated Wound Healing:
Individuals with diabetes, immunocompromised conditions, or peripheral vascular disease may experience impaired wound healing, predisposing them to chronic wounds and infections that can progress to gangrene. Managing complicated wounds requires a multidisciplinary approach, including wound care specialists, podiatrists, and infectious disease specialists. - Surgical Considerations:
Surgical management of gangrene in special populations may be challenging due to underlying medical conditions, such as diabetes, cardiovascular disease, or immunocompromised states. Surgical interventions, such as debridement or amputation, may carry higher risks of complications and require careful preoperative evaluation and optimization. - Infection Control:
Preventing and managing bacterial infections in immunocompromised individuals or those with diabetes is crucial for preventing the progression of gangrene. Antibiotic therapy may be necessary to treat underlying infections and prevent systemic spread. - Rehabilitation and Support:
Rehabilitation and support services play a critical role in the recovery and rehabilitation of individuals with gangrene, particularly those who undergo surgical interventions or amputations. Physical therapy, occupational therapy, and psychological support can help individuals regain function, mobility, and quality of life.
Prevention Strategies for Gangrene in Special Populations
Preventing gangrene in special populations requires a comprehensive approach addressing underlying risk factors and promoting healthy lifestyle habits:
- Management of Chronic Conditions:
Optimal management of chronic medical conditions, such as diabetes, peripheral arterial disease, and immunocompromised states, is essential for reducing the risk of gangrene. This includes regular monitoring, medication adherence, blood sugar control, and lifestyle modifications. - Foot Care and Monitoring:
Individuals with diabetes or peripheral neuropathy should practice daily foot care, including regular inspection of the feet for cuts, blisters, or signs of infection. Proper foot hygiene, wearing appropriate footwear, and avoiding injury are crucial for preventing foot ulcers and gangrene. - Smoking Cessation:
Smoking cessation is paramount for individuals at risk of gangrene, particularly those with peripheral arterial disease or diabetes. Smoking cessation programs and support services can help individuals quit smoking and reduce their risk of vascular complications. - Regular Medical Check-Ups:
Routine medical check-ups and screenings are important for early detection and management of conditions predisposing to gangrene, such as diabetes, peripheral arterial disease, and immunocompromised states. Regular monitoring of blood sugar levels, blood pressure, cholesterol levels, and vascular function can help identify and address risk factors. - Education and Awareness:
Educating individuals, caregivers, and healthcare providers about the risk factors, signs, and symptoms of gangrene is crucial for early detection and intervention. Promoting awareness of preventive measures, such as proper foot care, smoking cessation, and adherence to medical treatments, can help reduce the burden of gangrene in special populations.
Conclusion
Gangrene poses significant risks and challenges, particularly in special populations with specific medical conditions or lifestyle factors. Individuals with diabetes, peripheral arterial disease, immunocompromised conditions, trauma, or advanced age are at increased risk of developing gangrene and may encounter unique challenges in diagnosis, treatment, and management. Preventing gangrene in special populations requires a multidisciplinary approach addressing underlying risk factors, promoting healthy lifestyle habits, and providing education and support services. By raising awareness, implementing preventive measures, and optimizing medical care, we can reduce the burden of gangrene and improve outcomes for individuals in special populations.