Emerging Therapies And Research In Varicose Vein Management
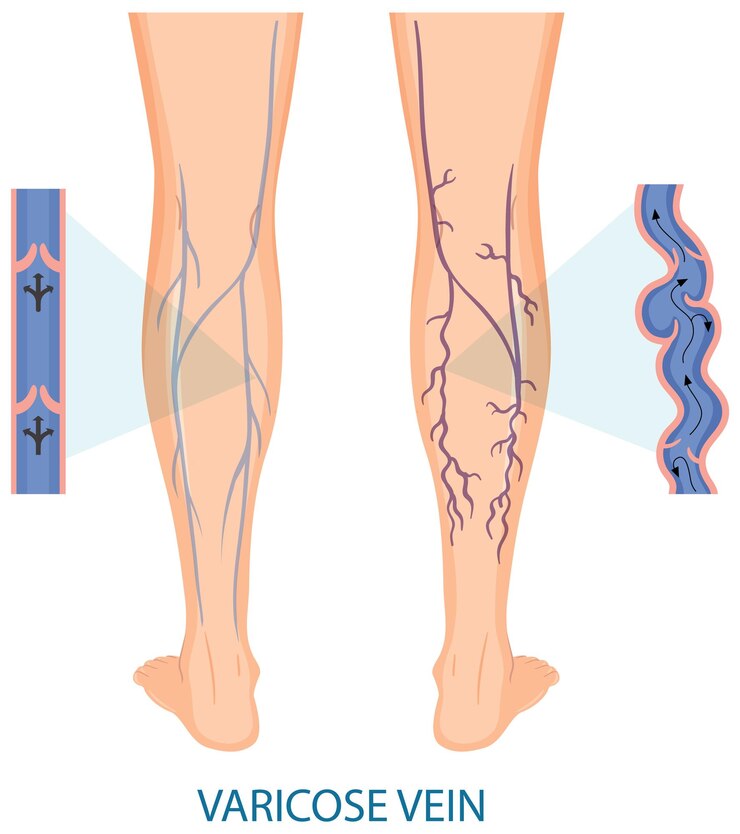
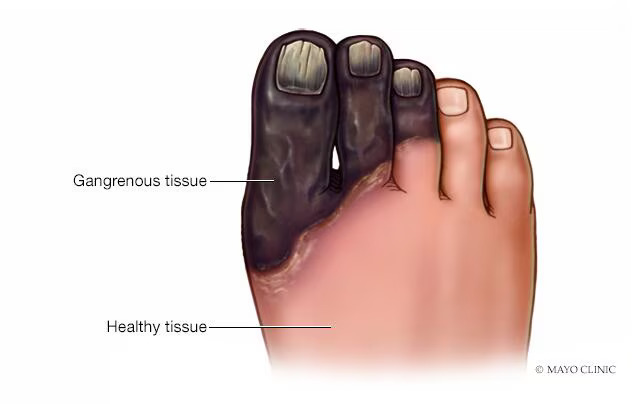
Varicose veins, characterized by twisted, enlarged veins that typically appear blue or purple, affect millions of people worldwide. While varicose veins are often considered a cosmetic concern, they can also cause discomfort, pain, and complications such as venous ulcers and thrombophlebitis. In recent years, advancements in medical technology and research have led to the development of novel therapies for varicose vein management. This article explores emerging therapies and research in varicose vein management, highlighting potential breakthroughs that may transform treatment approaches and improve patient outcomes.
Understanding Varicose Veins
Before discussing emerging therapies, it’s important to understand the underlying mechanisms and manifestations of varicose veins. Varicose veins occur when the valves within the veins become weakened or damaged, leading to inefficient blood flow and pooling of blood in the veins. This results in the characteristic bulging, twisted appearance of varicose veins, most commonly observed in the legs. Genetics, advancing age, obesity, pregnancy, and extended standing or sitting are risk factors for varicose veins.
Emerging Therapies
Endovenous Laser Ablation (EVLA):
Endovenous laser ablation (EVLA) is a minimally invasive procedure that involves inserting a laser fiber into the affected vein and delivering laser energy to seal the vein shut. This causes the vein to collapse and eventually be reabsorbed by the body, eliminating the varicose vein. EVLA offers several advantages over traditional vein stripping surgery, including less pain, faster recovery times, and lower risk of complications. Emerging research is focused on optimizing EVLA techniques and outcomes, including patient selection, laser parameters, and long-term efficacy.
Radiofrequency Ablation (RFA):
Another minimally invasive method used to treat varicose veins is radiofrequency ablation (RFA). It involves inserting a catheter with a radiofrequency electrode into the vein and delivering thermal energy to heat and close the vein. RFA is highly effective in treating varicose veins and has been shown to produce durable results with low rates of recurrence. Ongoing research is exploring novel RFA techniques, including catheter design, energy delivery systems, and combination therapies, to further improve treatment outcomes and patient satisfaction.
Foam Sclerotherapy:
Foam sclerotherapy is a minimally invasive procedure that involves injecting a foam sclerosant into the varicose vein to cause inflammation and closure of the vein. Foam sclerotherapy is particularly effective for treating smaller varicose veins and spider veins, offering a less invasive alternative to surgical interventions. Emerging research is focused on optimizing foam sclerotherapy techniques, including sclerosant concentration, foam stability, and injection volume, to achieve optimal outcomes while minimizing side effects.
Mechanochemical Ablation (MOCA):
Mechanochemical ablation (MOCA) is a relatively new technique that combines mechanical disruption of the vein wall with chemical sclerosis to close the varicose vein. This hybrid approach offers the advantages of both mechanical and chemical ablation while minimizing thermal injury to surrounding tissues. Early studies have shown promising results with MOCA, including high rates of vein closure and low complication rates. Further research is underway to evaluate the long-term efficacy and safety of MOCA compared to other varicose vein treatments.
Research Directions
Novel Sclerosants and Adjuvant Therapies:
Researchers are exploring novel sclerosants and adjuvant therapies to enhance the efficacy and safety of sclerotherapy for varicose vein management. This includes investigating alternative sclerosants, such as polidocanol and sodium tetradecyl sulfate, as well as adjunctive treatments, such as ultrasound-guided foam sclerotherapy and cryo-sclerotherapy. By optimizing sclerotherapy techniques and agents, researchers aim to improve treatment outcomes and reduce the need for invasive procedures.
Biomarkers and Predictive Models:
Advancements in biomarker research and predictive modeling hold promise for identifying patients at higher risk of varicose vein progression and complications. Researchers are investigating circulating biomarkers, genetic markers, and imaging features associated with varicose vein severity and prognosis. By developing predictive models and risk stratification tools, clinicians can better tailor treatment strategies and optimize patient outcomes in varicose vein management.
Patient-Centered Outcomes Research:
Patient-centered outcomes research aims to evaluate the impact of varicose vein treatments on patients’ quality of life, satisfaction, and functional outcomes. Researchers are conducting studies to assess patient-reported outcomes, including pain, mobility, cosmetic appearance, and psychosocial well-being, following different varicose vein interventions. By incorporating patient preferences and perspectives into treatment decision-making, clinicians can improve patient engagement and adherence to treatment recommendations.
Conclusion
Advancements in varicose vein management are revolutionizing the field of vascular medicine, offering new minimally invasive options for patients with symptomatic varicose veins. From endovenous ablation techniques to foam sclerotherapy and mechanochemical ablation, emerging therapies hold promise for improving treatment outcomes, reducing complications, and enhancing patient satisfaction. Ongoing research efforts in biomarker discovery, predictive modeling, and patient-centered outcomes research aim to further optimize varicose vein management and improve the overall quality of care for affected individuals. By embracing innovation and collaboration, clinicians and researchers can continue to advance the field of varicose vein management and ultimately improve the lives of patients with this common vascular condition.